Abstract
Introduction
The increasing use of alternative donors has expanded allogeneic hematopoietic stem cell transplantation (HSCT) eligibility in patients with acute myeloid leukemia (AML) without HLA-identical siblings (matched-SIB). However, optimal donor selection remains controversial and current practice is largely based on transplantation centres' experience. Unrelated donor (URD) HSCT is associated with longer waiting times to transplantation than umbilical cord blood or haploidentical HSCT, but the impact of HSCT delays on transplantation rates and survival outcomes is unclear in this setting. In this study we evaluated the performance of a donor selection algorithm consisting in the allocation of patients with AML without matched-SIB to fully matched (8/8) or mismatched (7/8) URD.
Methods
Retrospective analysis including adult patients with AML who received approval for first-time allogeneic HSCT with myeloablative conditioning at our institution between January 2011 and February 2017. Matched-SIB was the preferred donor choice for all patients. Fully matched (8/8) or mismatched (7/8) URD were selected through high-resolution HLA-A, HLA-B, HLA-C and DRB1 typing for those patients without an available matched-SIB. Non-parametric cumulative incidence and Kaplan-Meier estimates were obtained to assess transplantation and overall survival (OS) rates, respectively. Fine-Gray competing risks regression was used to identify predictors of failure to reach transplantation. Age, intention-to-treat (ITT) and disease status at the time of transplantation approval were included in the multivariate analysis.
Results
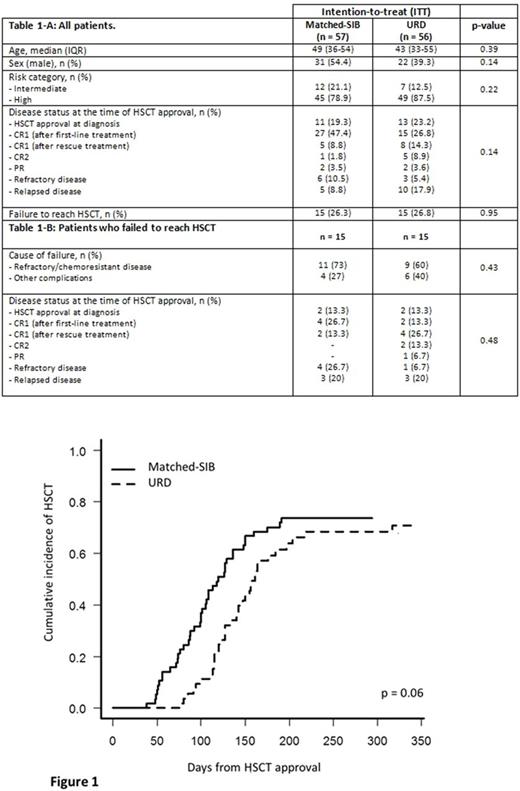
Table 1 summarizes the characteristics of the 113 eligible patients during the study period. Fifty-seven patients (50.4%) were allocated to a matched-SIB donor, whereas URD search was started in the remaining 56 patients (49.6%) without an available matched-SIB. Thirty patients (26.5%) failed to reach transplant after the approval to undergo transplantation. Figure 1 shows the cumulative incidence functions of transplantation from time of approval (Gray's p = 0.06). The estimated probabilities to reach transplantation were 74% and 71% for patients with or without a matched-SIB donor. Median time to HSCT from transplantation approval was shorter in patients with a matched-SIB donor (100 versus 136 days). Disease status at the time of transplantation approval was the only predictor of failure to reach transplantation in the multivariate analysis (sHR for any disease status versus CR1 = 1.69, p = 0.04). The 3-year OS from time of transplantation approval in the ITT population was 35% (28% versus 41% for patients with or without a matched-SIB donor, respectively; log rank p = 0.39), while the 3-year OS from time of transplantation was 46% (46% versus 54% for patients who underwent a matched-SIB HSCT or an URD HSCT, respectively; log rank p = 0.46).
Conclusions
8/8 or 7/8 URD selection in patients with AML without an available matched-SIB led to increased times to transplantation but did not have an impact on the probability of failure to reach transplantation and did not result in inferior survival outcomes in comparison with patients with a matched-SIB.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal